Why Partial Coverage? Rethinking the Full Crown
Jun 27, 2025
Why Partial Coverage? Rethinking the Full Crown
By Dr. Steve Schiffenhaus, DMD | The BAARD Institute
The days of defaulting to full-coverage crowns are numbered—and for good reason.
At The BAARD Institute, we champion a different approach: partial coverage ceramics grounded in a biologically centered, minimally invasive, and adhesive protocol. Why? Because modern restorative dentistry isn’t just about fixing teeth, it’s about preserving them for the long haul.
Let’s break down why partial coverage restorations, particularly bonded overlays and onlays, represent the future of restorative design.
Crowns: A Legacy of Mechanical Retention
Traditional crown preps date back to the early 20th century, built around the assumption that retention must come from friction and sidewalls, not chemistry. But this comes with a biological cost: significant removal of healthy tooth structure, increased stress on the pulp, and the risk of catastrophic failure when things go wrong.
-
Even well-sealed luted crowns exhibit microleakage under cyclic load, allowing bacterial ingress over time¹.
-
Long-term studies show 10–15% pulpal failure rates for luted metal crowns².
-
And with every millimeter of dentin lost, the tooth’s fracture resistance drops sharply³.
This isn’t ideal, it’s outdated.
Adhesion Changes Everything
Thanks to advancements in adhesive dentistry, we’re no longer limited to hat-like caps that rely on mechanical grip. Bonded ceramics allow us to rethink everything: retention, stress distribution, preparation design, and long-term outcomes.
What do we gain?
✅ More conservative preps that preserve dentin and enamel
✅ Better fracture resistance of both tooth and restoration
✅ Higher long-term pulp vitality, especially when paired with techniques like Immediate Dentin Sealing (IDS)⁴
Not All Failures Are Equal
One of the most powerful ideas we teach at the BAARD is that failures are inevitable but some are better than others.
A bonded onlay that debonds cleanly and can be re-cemented is vastly preferable to a crown that cracks a tooth down the root. Our biologic goal is to ensure that if something fails, the restoration fails, not the tooth⁵.
That’s a complete paradigm shift—from “how long will the crown last?” to “how long can I keep this tooth alive?”
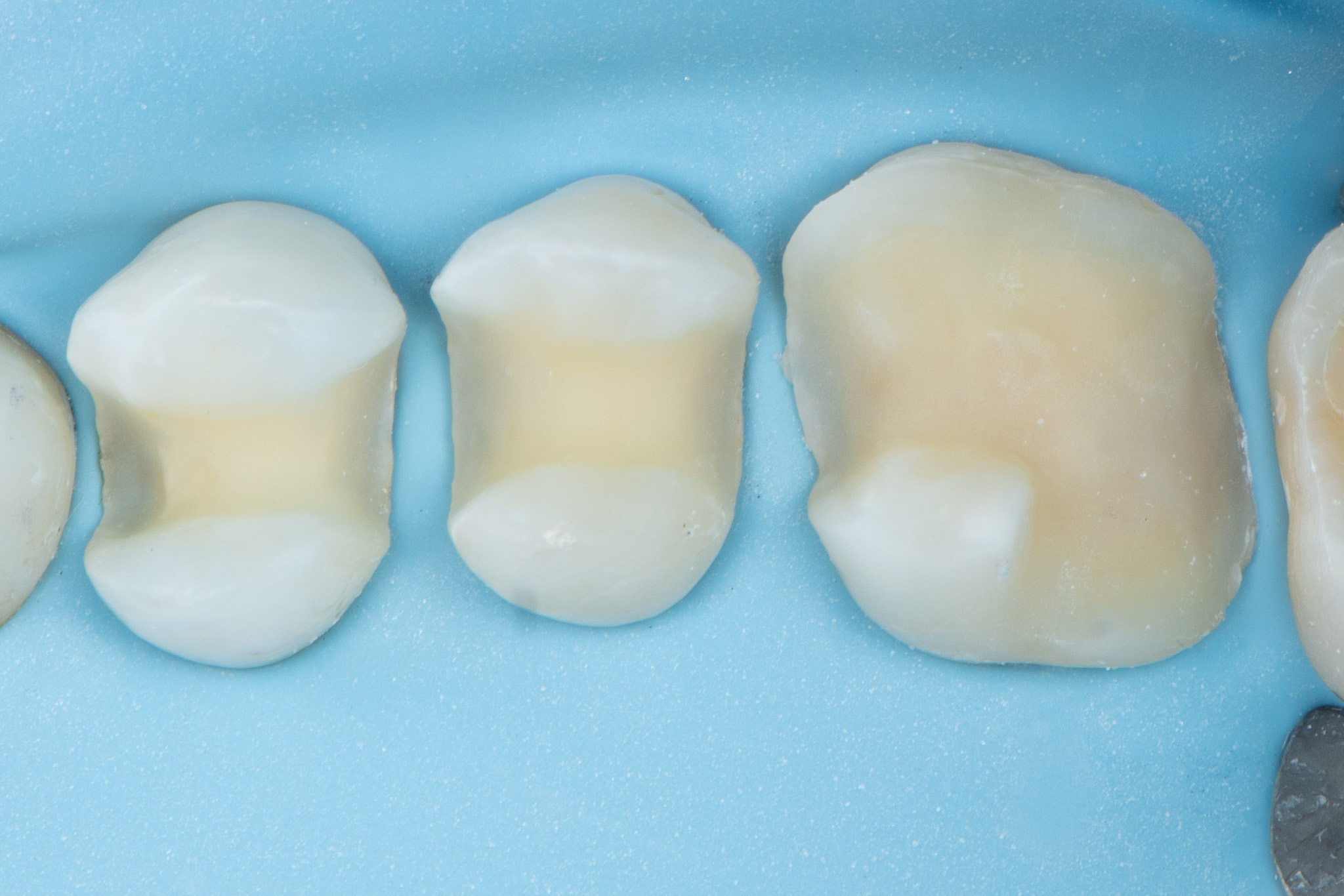
The Compression Dome: Nature’s Design
The natural tooth is a biomechanical masterpiece. Enamel and dentin form a graded composite system designed to withstand enormous compressive forces up to 1200 N in some individuals—without catastrophic failure⁶.
But this only works when the integrity of the compression dome is preserved. When we cut into that system (especially in the central fissure or cervical region), we concentrate tensile forces in areas ill-equipped to handle them⁷.
➡️ The result? Cracks.
➡️ The solution? Preserve and reinforce the compression dome with bonded ceramics that mimic enamel’s modulus of elasticity⁸.
When to Cover Cusps—and When Not To
So when do you need to cover cusps?
-
Endodontically treated teeth
-
Oblique fractures under cusps
-
Extensive cracks or vertical fractures
-
Cusp undermined by large restorations or wear
But in many cases, especially with proper bonding and a structurally sound base, you don’t need full occlusal coverage. This is where materials like e.max (lithium disilicate) shine thin yet strong, and ideal for preserving enamel while sealing and stabilizing the tooth⁹.
The Evidence Is Clear
Studies consistently show better long-term outcomes with bonded partial coverage:
-
95% pulp vitality at 7 years for cracked teeth restored with bonded overlays¹⁰
-
Partial coverage glass ceramics outperform crowns in fracture resistance over 10+ years¹¹
-
Microleakage is dramatically reduced with bonded ceramics vs luted crowns¹²
-
Biomimetic designs reduce stress and improve fatigue resistance¹³
Key Takeaway: Preserve What You Can, Bond What You Must
The full crown isn’t going extinct
…but it should no longer be the gold standard.
For many posterior restorations, it’s an overtreatment with a steep biologic cost especially when better adhesive alternatives exist.
Even Shillingburg acknowledged this over 40 years ago:
“This does not mean that a full veneer design must be used on every tooth. Instead, it should be used on those teeth whose restoration demands maximum retention... Full coverage in the right circumstance can be excellent treatment, but it is overused.”
— Herbert T. Shillingburg, DDS, Fundamentals of Fixed Prosthodontics, 3rd Ed., Ch. 10
He went on to cite insurance data showing 93% of cast restorations in 1979 were full coverage, concluding that the percentage would likely be even higher today.
We agree with his core message: full coverage should be the exception not the rule.
Partial coverage ceramics, when bonded correctly, offer strength, longevity, and a chance to preserve the most important element: the patient’s natural tooth.
At The BAARD Institute, we teach you how to do just that.
👇 Want to Go Deeper?
Our full Overlay & Onlay course available online or in person covers the exact clinical techniques, preparation designs, and adhesive workflows discussed here.
Learn how to preserve more teeth with bonded, biomimetic restorations that last.
👉 Explore the In-Person Course
👉 Explore the Online Course
Bonus: You’ll get access to our free Immediate Dentin Sealing protocol just by visiting the page.
References
-
Khvostenko D, et al. Cyclic mechanical loading promotes bacterial penetration along composite restoration marginal gaps. Dent Mater. 2015;31(6):702–10.
-
Reuter JE, et al. The longevity of crowns and the frequency of pulp deaths. J Oral Rehabil. 1984;11(4):373–80.
-
Larson TD, Douglas WH, Geistfeld RE. Effect of prepared cavities on the strength of teeth. Oper Dent. 1981;6(1):2–5.
-
Hofsteenge JW, et al. Effect of immediate dentine sealing on aging and fracture strength of lithium disilicate inlays and overlays. J Mech Behav Biomed Mater. 2020;110:103906.
-
Kaka M, et al. Outcomes of cracked teeth treated with bonded restorations. J Esthet Restor Dent. 2022;34(2):243–250.
-
Chai H, et al. Remarkable resilience of teeth. PNAS. 2009;106(18):7289–93.
-
Magne P, Belser UC. Shape and stress distribution in posterior teeth: a finite element study. Int J Periodontics Restor Dent. 2002;22(5):425–33.
-
Ausiello P, et al. Class II restorations incorporating ceramic and composite materials: stress analysis via FEA. Dent Mater. 2017;33(12):1456–65.
-
Lubauer J, et al. Fracture toughness of lithium disilicates. Dent Mater. 2022;38(2):318–32.
-
Opdam NJM, et al. Survival of cracked teeth restored with bonded restorations. Oper Dent. 2007;32(6):593–600.
-
Morimoto S, et al. Survival rate of all-ceramic restorations: meta-analysis. J Dent Res. 2016;95(5):543–49.
-
Tjan AH, et al. Microleakage of cast gold crowns bonded with Panavia vs zinc phosphate. J Prosthet Dent. 1992;67(1):11–17.
-
Gomes de Carvalho AB, et al. Mechanical behavior of different onlay prep designs in endo-treated molars. Materials. 2021;14(8):1923.